Diabetic Retinopathy is a serious eye disease caused by diabetes that can result in loss of vision and blindness. It is one of the most common topics asked in FMGE and NEET-PG
- Duration of diabetes is the most important risk factor.
- In 10 years, 20% of type 1 and 25% of type 2 diabetics develop DR.
- In 20 years, 90% of type 1 and 60% of type 2 diabetics show signs of DR.
- In 30 years, 95% of both type 1 and type 2 diabetics develop DR.
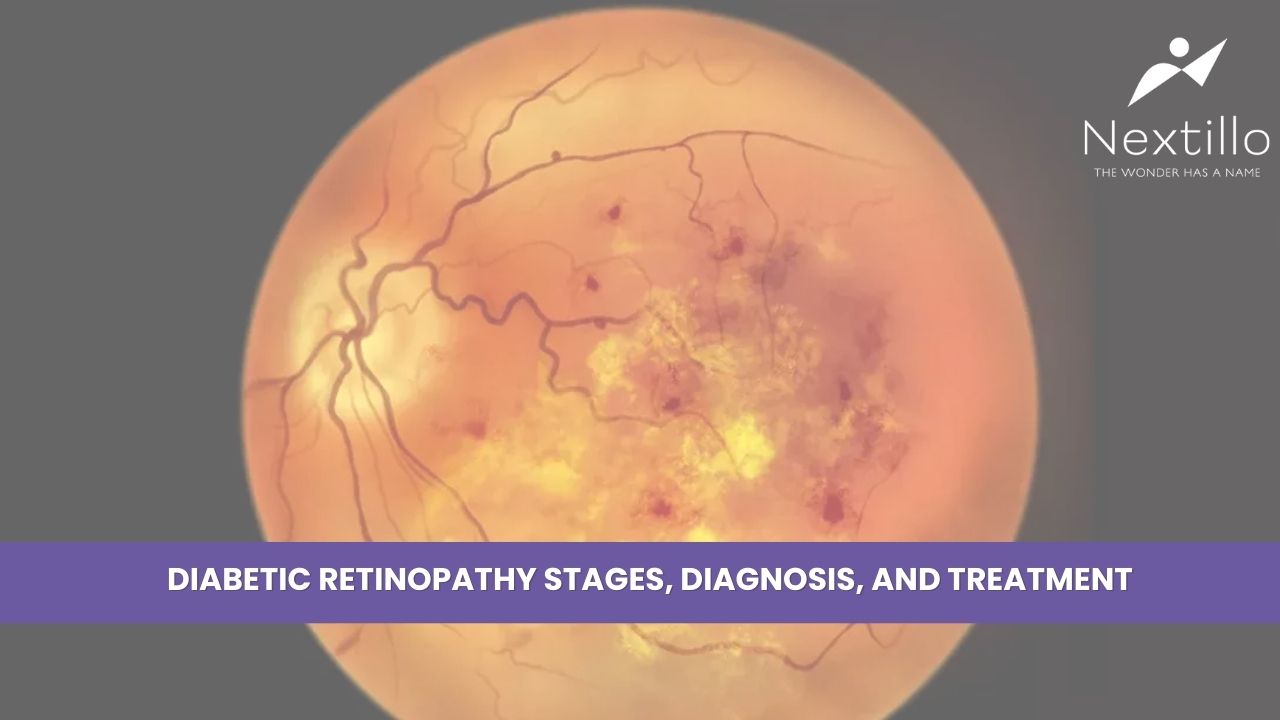
What is Diabetic Retinopathy?
Diabetic retinopathy occurs when blood glucose levels remain so high, causing damage to the small retinal blood vessels. Long term, it can affect vision through inflammation, leakage of fluid, and formation of new vessels.
PATHOGENESIS
- Microangiopathy leading to hypoxia and retinitis proliferans.
- Vascular leakage, causing retinal edema, hemorrhages, and hard exudates.
- Formation of new blood vessels (neovascularization) due to ischemia.
Stages of Diabetic Retinopathy
- Mild Nonproliferative Retinopathy
In the first phase, small regions of ballooning of the retinal blood vessels (microaneurysms) occur. They leak fluid but do not affect vision. In most people with this phase, there are no symptoms, but it can be found during routine eye examinations. In this stage, the disease is not serious and can be left untreated, but regulation of blood sugar prevents the progression.
- Moderate Nonproliferative Retinopathy
In the second stage, the damage to the blood vessels is more extensive. Part of the vessels becomes blocked, and the blood cannot travel to the retina in such areas. This decreased oxygenation of the retina predisposes the retina to damage. In this stage, patients notice some changes in vision. Regular follow-up on a regular basis by an ophthalmologist is recommended in order to prevent worsening of the condition.
- Advanced Nonproliferative Retinopathy
In this phase, more blood vessels are blocked, and there is a severe deficiency of oxygen within the retina. The retina forms new, immature blood vessels to compensate for the poor oxygenation. New blood vessels are fragile and prone to leaking blood into the retina. Patients experience difficulties with their vision, like blurry vision, night blindness, or dark spots in their eyes.
- Proliferative Diabetic Retinopathy (PDR)
The most advanced type of diabetic retinopathy, proliferative diabetic retinopathy, is when the retina forms new, abnormal blood vessels. These are extremely fragile blood vessels and susceptible to leakage and blinding. The new tissue can be generated, which can make the retina detached and hence lead to irreversible loss of vision. Proliferative diabetic retinopathy needs immediate medical care to avoid permanent damage.
Read more: Ophthalmology Blogs for Fmge and Neet PG Preparation
Diabetic Maculopathy
It involves changes in the macular region affecting central vision.
Diagnosis
Fluorescein Angiography
Dye is infused through a vein in the arm, and a camera captures an image of the retina as the dye flows through the blood vessels.
Optical Coherence Tomography (OCT)
OCT is a non-invasive imaging procedure that uses light waves to give detailed cross-sectional views of the retina. OCT can detect inflammation or leakage of fluid in the retina.
Treatment of Diabetic Retinopathy
Although diabetic retinopathy is a serious condition, it can be treated and managed adequately by early detection and control. The treatment aims at avoiding further loss of vision, preserving vision, and, in some cases, recovering lost vision. Some of the most common management methods are
- Control of Blood Sugar Level
The key to managing diabetic retinopathy is to manage blood sugar levels.
- Laser Treatment (Photocoagulation)
In advanced diabetic retinopathy, lasers are used to seal leaking vessels and prevent further leakage. It can be done, especially in advanced diseases, for example, proliferative diabetic retinopathy.
- Intravitreal Injections
In certain cases, the medications are injected into the eye. They include anti-VEGF drugs like bevacizumab that block new blood vessel formation and corticosteroids to reduce inflammation and swelling.
- Vitrectomy Surgery
For complications such as excessive bleeding or retinal detachment, surgery called vitrectomy is required. Removal of the gel-like vitreous that may have blood and replacing it with clear fluid.
Prevention
Prevention of diabetic retinopathy requires the careful management of diabetes and leading a healthy lifestyle-
- Manage blood sugar levels Have normal blood pressure and cholesterol to avoid further injury to the blood vessels by diet, exercise, and drugs.
- Diabetic patients should maintain regular exercise (6 times a week) and a healthy diet and avoid smoking and alcohol.
- Regular eye tests, even without symptoms, are necessary in order for retinal changes to be noted in their early stages.
Crack the FMGE Exam with Confidence—Download the Nextillo App Now on iOS & Android!”





1 Comment
Sahil medicos
Great insights! This blog does an excellent job of simplifying complex medical concepts , making it easy for students and prof alike. Looking forward to more such informative content..